Abstract
Autologous Stem Cell Transplantation (ASCT); is a universal accepted therapy for rescuing relapsed Hodgkin (HL) and non-Hodgkin (NHL) lymphoma patients and for consolidation of mantle cell lymphoma (MCL). The most used preparative regimens in this setting are BEAM and CBV. both of them include carmustine, a medication with serious shortage and cost problems, therefore , is very important to find alternative regimens. During the nineties the combination of high dose of carboplatin plus cyclophosphamide and etoposide (CEC) was explored, however, it was abandoned due to high toxicity. We present our experience with 108 patients using this regimen but with intermediate dose of carboplatin (Inter CEC)
Methods:
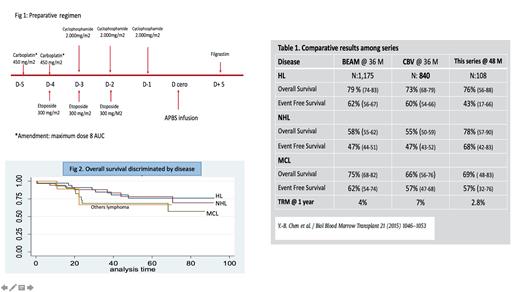
We did a retrospective descriptive longitudinal observational study. All consecutive patients who met the inclusion criteria; age above 18 years, diagnosis of HL, NHL, M CL, and transplanted with Inter CEC were included. The preparative regimen consisted of carboplatin 900 mg/m2, etoposide 900 mg/m2, and cyclophosphamide 6.000 mg/m2, split in five days (fig 1). All patients received peripheral blood stem cells, and from d + 5 until neutrophil recovery, daily filgrastim. Every patient signed informed consent and the study was approved for institutional ethical committee.
Results:
From Oct 2013 to May 2020, 108 patients were included; median age was 45 years (18-70), 43.5% were female, 20% were older than 60 years and 79.6% had advanced disease at diagnosis. Thirty-five (32.4%) had HL, 35 (32.4 %) NHL (28 diffuse large B cell, 7 follicular), 29 (26,9%) had MCL, and 9 (8.3%) had other lymphomas. 34% of HL patients and 48% of cases were transplanted in CR1 after being refractory to first line therapy, while 44% and 14% of HL and NHL respectively had active disease at the time of transplantation. Regarding MCL cases; 21 (72,4%) had MIPI above 3 points and 96.5% were transplanted in first remission.
All of the evaluable patients at day + 30 had hematopoietic recovery, median time to achieve 500 neutrophil /ul or more was 12.3 days (10-30) and for self-sustained platelet counts, 20.000/ul or more, was 15.3 (10-34).
After a median follow up for surviving patients of 42,2 months the overall survival (OS) (Kaplan-Meier) at 48 months for the entire group was 74% (CI 63-82) and the event free survival (EFS) was 57% (CI 43-69). When the OS and EFS were discriminated for diseases, it was; for HL 76% (CI 56-88) and 43% (CI 17-66), for NHL 78% (CI: 57-90) and 68% (CI 42-83), and for MCL 69% (48-83) and 57% (CI 32-76) respectively (Fig 2). Eleven out of 18 patients (61%) transplanted with active disease achieved complete remission and 14 out of the entire group relapsed during the first years of transplant
The transplant related mortality (TRM) at 1 year was 2.8%, the relapse associated deaths were 13% and, in 5 patients, who died after one year of transplant, the cause was not found. The main toxicity was mucositis; 46%, (grade II-IV: 22%), 30 patients (28%) had confirmed infections; bacteremia 17 cases, pneumonia 5, and others infections 6. Renal toxicity occurred in 24 cases (22%), grade 1; 15.8%, grade 2; 4.6% and grade 3; 1.8%
Discussion
Comparing results among trials is always difficult; however, despite that, in our series 58% of the cases were transplanted with active disease, our outcomes compare favorably with the results informed after the use of BEAM or CBV presented by CIBMTR in the largest trial published so far (table 1). The use of intermediate dose of carboplatin plus etoposide and cyclophosphamide produces a very good control of the lymphoma activity with acceptable toxicity, and achieves good OS and EFS. Other advantage of this regimen is that is carmustine free. The next step in our study is to do a matched paired analysis with patients transplanted with BEAM or CBV
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal